Insulin Resistance 101

Insulin Resistance (IR), also known as Metabolic Dysfunction or Prediabetes, is when cells in the body stop responding to insulin and lose their ability to metabolize glucose. The body is unable to regulate blood sugar. IR is a serious condition and should not be ignored. It can be reversed if caught early. A fasting blood sugar greater than 100 mg/dL indicates that IR may be present.
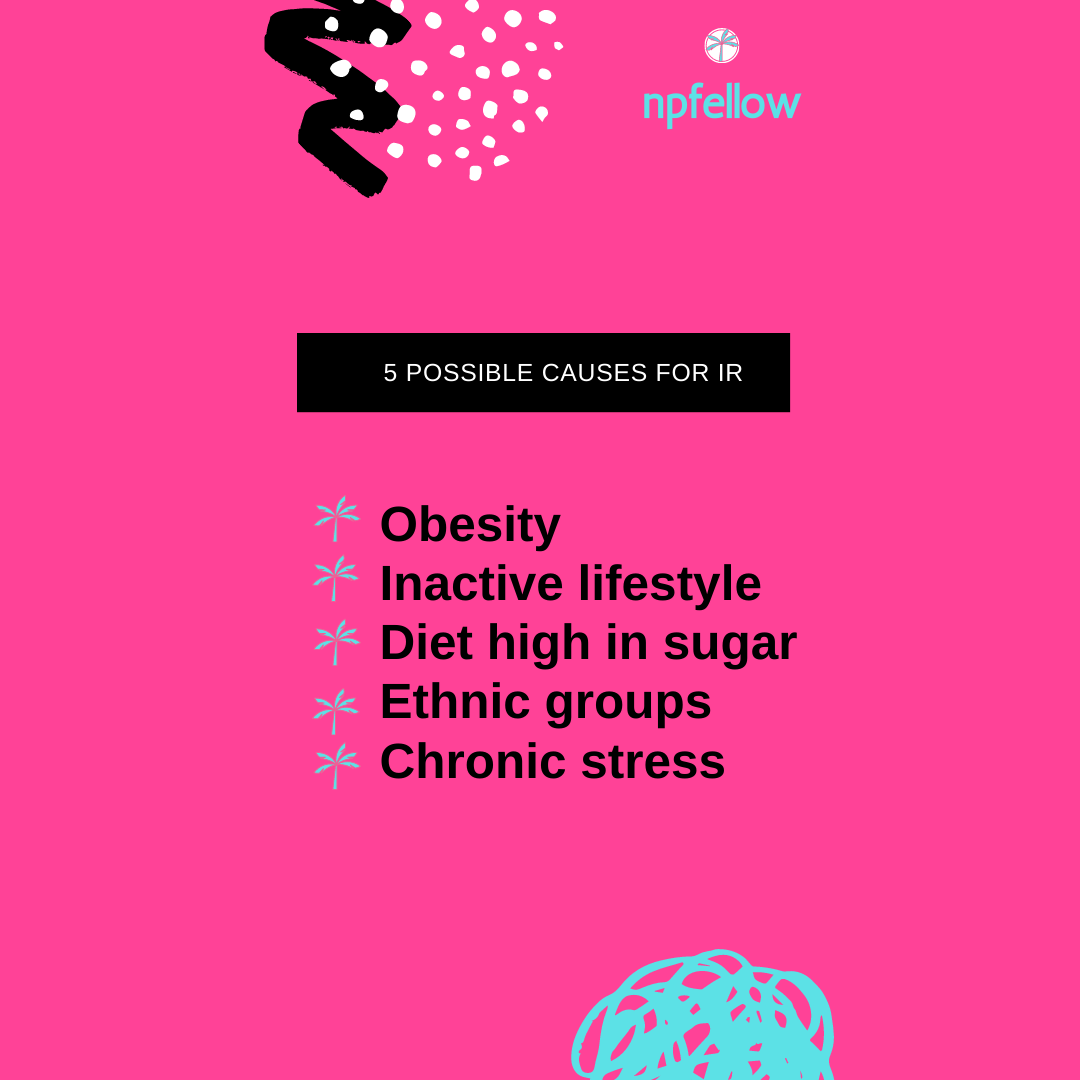
Two key components to IR include an altered response to insulin signaling and an increased amount of insulin in the blood. The cells become desensitized to insulin. They become immune to the increased circulating insulin and stop responding. The second problem is hyperinsulinemia. Not only do cells stop responding, organs like, the ovaries, bask and thrive in this excess insulin leading to hormonal imbalances. Increased insulin leads to facial hair and central adiposity in women, and breasts and loss of facial hair in men.
Awareness of IR is very important because it is at the center of aging and promotes the start of the chronic low-grade inflammation cascade. When the body loses its ability to metabolize and regulate glucose, waist adiposity is created and can become “toxic.” This central belly fat turns into a dynamic hormonal immune organ. This alters the immune response and drives inflammation throughout the entire body down to the inner lining of blood vessels. Oxidative stress occurs and arteries become hardened and inflamed. This how IR can lead to high blood pressure and lay the foundation for chronic disease.
IR Statistics
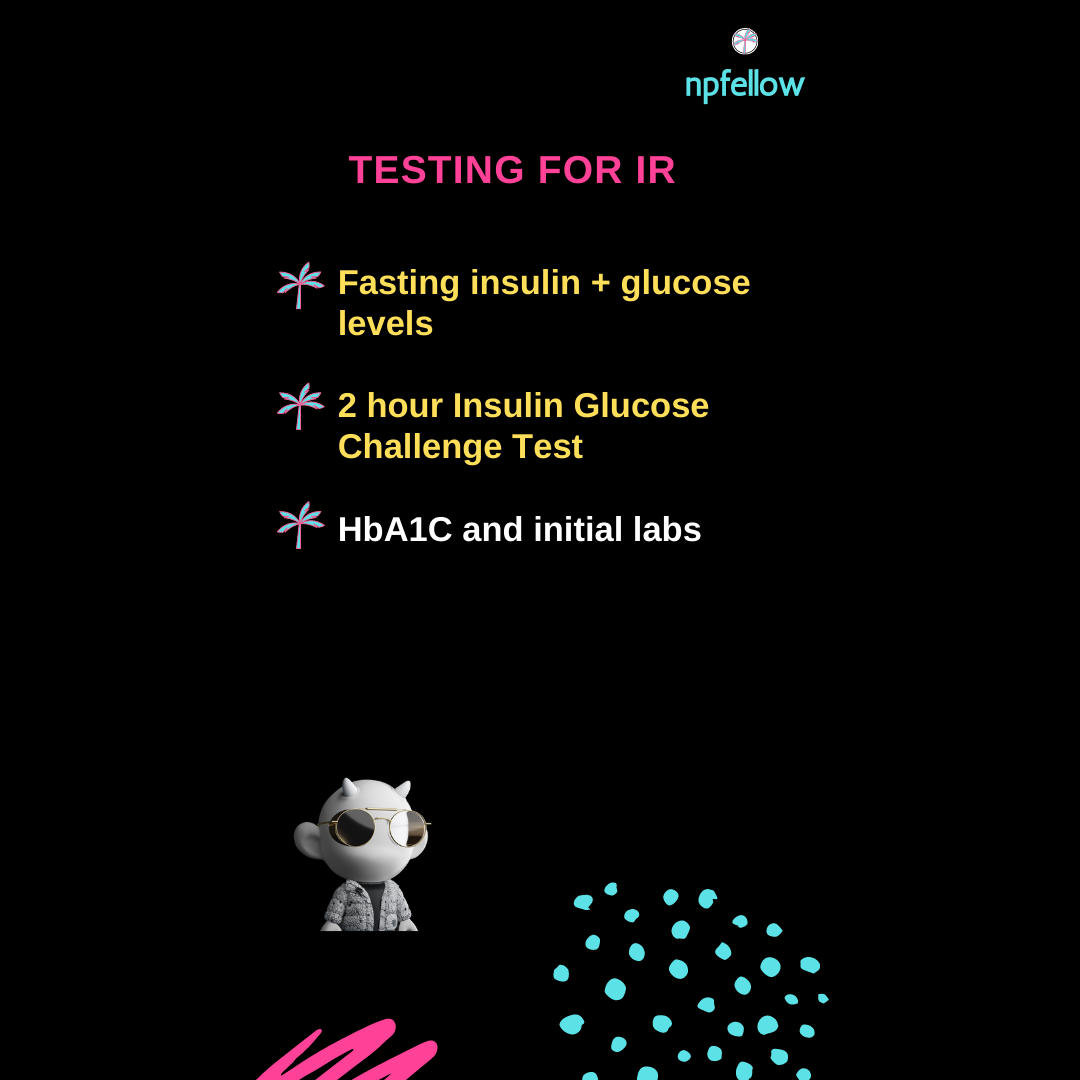
IR affects both adults and children. 1 in 2 Americans are insulin resistant and 90% are undiagnosed. IR is missed because most lab testing only includes blood glucose levels, and not actual insulin levels. The key here is to check both blood glucose and insulin levels. IR is a slow and steady path. In the early stages of IR blood sugar levels can be normal. This is because the body is compensating for high blood glucose levels by increasing insulin production. The insulin level also needs to be assessed. This is to check for an increased insulin level and any compensation by the pancreas. In the later stages of IR, cells stop responding to insulin and blood sugar rises. Both blood glucose and insulin levels will be elevated. This is finally when the lab testing picks up on the blood sugar imbalance.

IR Signs + Symptoms
It is important to note realize that IR can be silent; it produces no symptoms. Most people are unaware they are insulin resistant. Symptoms of IR include visceral belly fat, skin pigmentation changes in skin folds, fatigue after meals, high triglycerides, low HDL cholesterol, sugar cravings, and blood clotting problems.
When cells are not able to metabolize glucose as fuel they start to starve. The brain and body literally starve to death even though the person is eating. Belly fat increases and the brain starts to shrink. This starts the path of cognitive dysfunction- brain fog, depression, and memory loss.
IR Dx + Testing
IR is defined as a fasting blood sugar greater than 100 mg/dL, or a hemoglobin A1C of 5.7-6.4%. Testing for IR should include fasting blood glucose and insulin levels, a 2 hour glucose insulin tolerance test, hemoglobin A1C, and initial comprehensive lab testing. A fasting blood sugar of 126 mg/dL or greater, or a hemoglobin A1C of 6.5% or greater is indicative of Diabetes Mellitus Type 2.
IR Prevention + Management
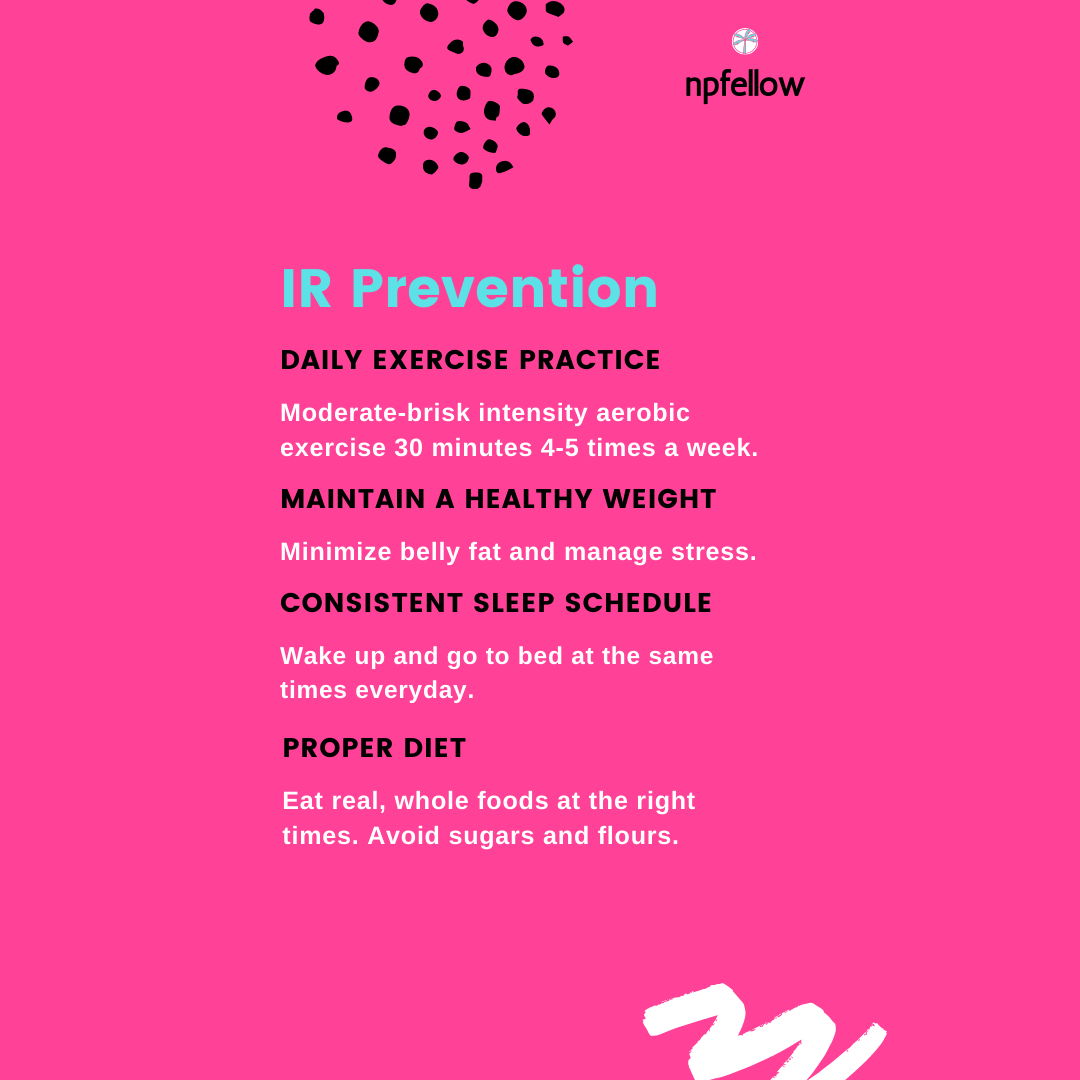
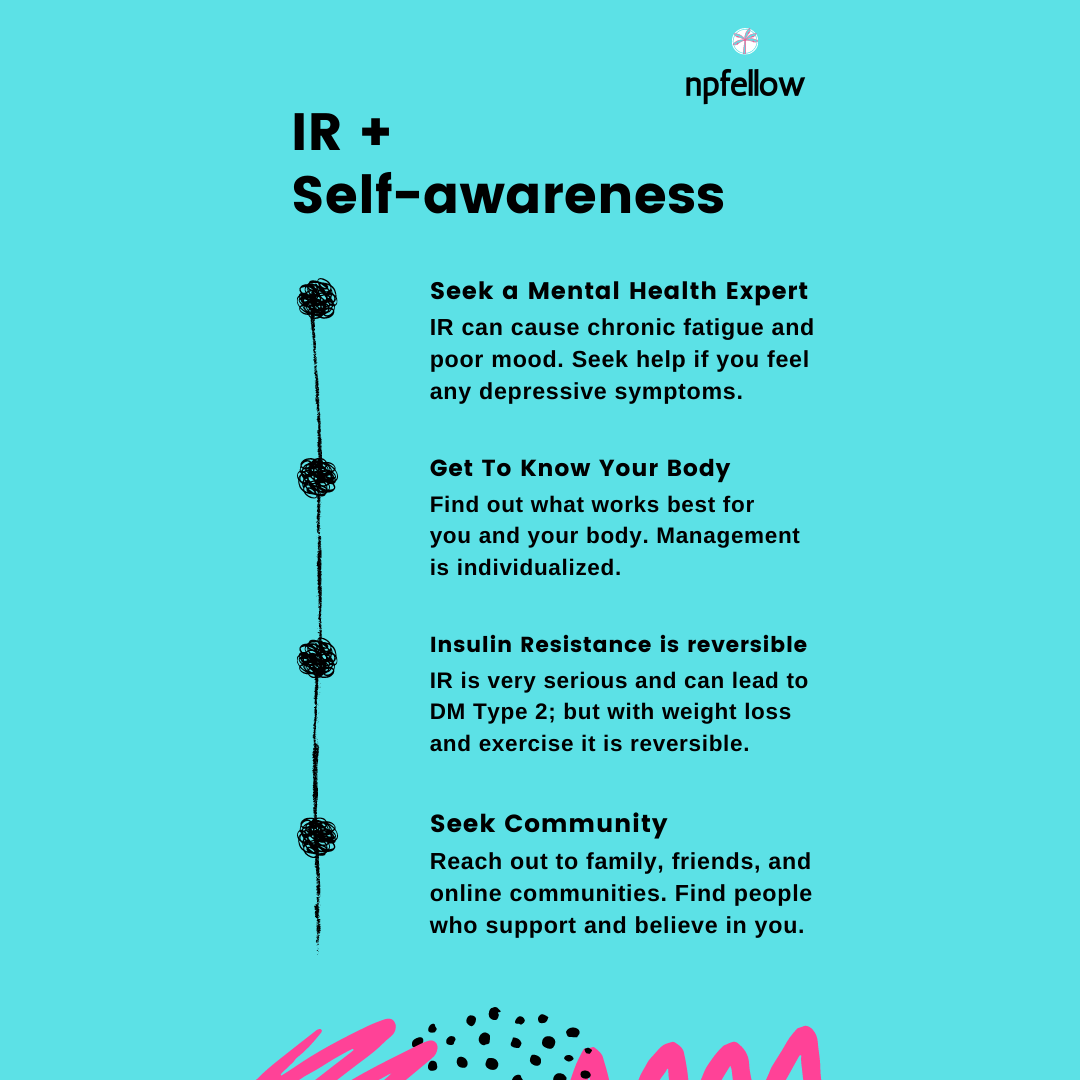
Prevention for IR consists of diet and lifestyle modifications. The perfect “prescription” for the insulin resistant is daily moderate-intense exercise for at least 30 minutes. Management is individualized. A personalized nutrition and exercise regimen should be followed. The goal is to lose weight- lose that central belly fat and increase insulin sensitivity. Weight loss can reverse insulin resistance. Time-restricted eating, exercise, and high-quality consistent regular sleep are critical for boosting insulin sensitivity. Movement drives glucose from the bloodstream into the cells to use as fuel. A regular sleep schedule syncs our circadian rhythm and normalizes insulin and cortisol hormone levels. Avoid eating late at night. This is the master key when it comes to diet. An optimal diet consists of high-quality protein, ancestral fats, and fruits and vegetables. Avoid floury, sugary, starchy, highly-processed foods. A diet rich in fiber is crucial for digestion and blood sugar homeostasis.
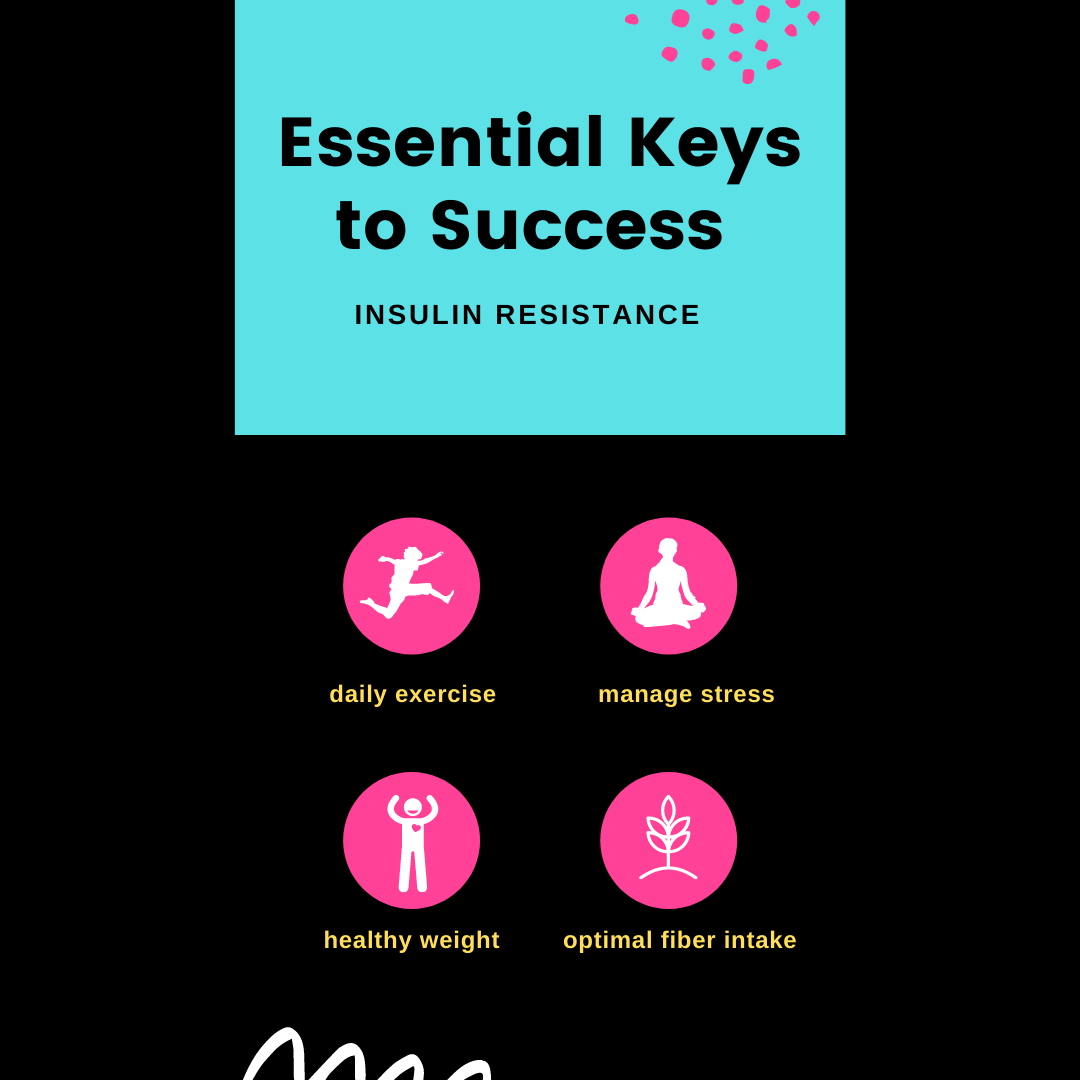
Keys to Success
The absolute key to success in IR prevention is to have a fasting insulin level less than 5. This demonstrates that insulin sensitivity is present. Another key element to success is eating low-glycemic, whole real foods. Getting in some form of movement or exercise daily along with 8 hours of sleep promotes healthy hormone levels. Adequate water and fiber intake support optimal digestion and blood sugar regulation.
Final Thoughts
Insulin resistance (IR) does not happen overnight. It is a gradual process that leads to rapid, premature aging. It is the precursor to Diabetes Mellitus Type 2. IR is a serious problem that needs to be addressed. It is our responsibility to take charge of our own health. We have the right to be healthy and live an abundant life.
Keep track of your diet, workouts, feelings and any changes you experience in a journal. Notify your primary healthcare provider of any new weight gain, excessive thirst or hunger, fatigue after meals, and sugar cravings. Visit your primary provider for a physical exam and lab testing yearly. Be mindful- don’t eat before bed, don’t drink your calories, and realize that IR is preventable and reversible.
Thank you for reading this post.
